Empowering Insights Into IVF & Cancer‑Related Fertility Challenges
Facing cancer brings emotional and physical hurdles—one of the most delicate being fertility. Fortunately, IVF and related fertility preservation techniques provide hope and control in uncertain times. This detailed, human-centered guide (over 1,200 words) explores the history, facts, FAQs, timeline, significance, daily-life impact, observance, wishes, and societal importance of IVF in the context of cancer.
- 🧬 What Is IVF & Why Is It Crucial in Cancer Care?
- 📜 History & Evolution
- 📌 7 Facts You Should Know
- ❓ Frequently Asked Questions
- ⏳ Timeline: From Conversation to Creation
- 🏠 Impact on Daily Life
- 🌍 Societal Significance
- 🎉 Wishes to Those Facing This Journey
- 🧠 Observations & Best Practices
- ✅ Conclusion: Fertility Tools in Cancer Care Are Empowering
🧬 What Is IVF & Why Is It Crucial in Cancer Care?
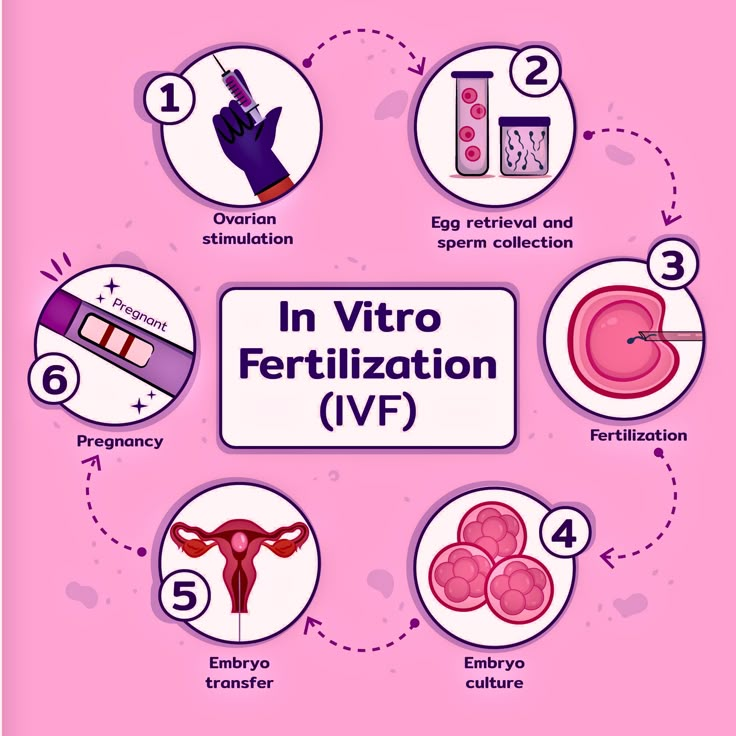
In-vitro fertilization (IVF) involves retrieving eggs or sperm, fertilizing them in a lab, and implanting embryos in the uterus. While often associated with overcoming infertility, IVF is also vital for fertility preservation in cancer patients—a proactive way to maintain the possibility of parenthood before treatment begins drjayanam.com+13mayoclinic.org+13rscbayarea.com+13.
📜 History & Evolution
Mid–20th century: Egg freezing (oocyte cryopreservation) was first developed for cancer patients, later becoming more mainstream cancer.org.
Late 20th century: IVF expanded from treating infertility to enabling planned parenthood amid disease and aging .
Early 21st century: Integration of reproductive medicine and oncology led to oncofertility, a specialized field offering fertility preservation to cancer patients before treatments harm reproductive organs academic.oup.com+2cancer.org+2jamanetwork.com+2.
2020s: Techniques like ovarian transposition, cryopreservation, and stem‑cell research advanced, especially for pediatric patients .
📌 7 Facts You Should Know
IVF is a key fertility preservation method
Eggs, embryos, or ovarian/testicular tissue can be frozen prior to cancer treatment cancer.org.Not all IVF is for post-cancer use
It also addresses conditions like blocked fallopian tubes or sperm issues cancer.org+15mayoclinic.org+15rscbayarea.com+15.Age and ovarian reserve matter
Younger patients tend to have better outcomes; cancer patients often rush the process pre-treatment arxiv.org+1thetimes.co.uk+1.Egg-freezing began as cancer care
Initially developed to preserve the fertility of cancer patients, it’s now widely used by women for fertility security academic.oup.com+14theaustralian.com.au+14drjayanam.com+14.IVF procedure carries physical risks
These include ovarian hyperstimulation, retrieval complications, and emotional strain theaustralian.com.au+5apnews.com+5pubmed.ncbi.nlm.nih.gov+5.Cancer itself—and fertility drugs—don’t clearly raise cancer risk
While underlying infertility is linked to higher uterine and ovarian cancer risk, IVF drugs haven’t shown solidly elevated cancer rates thelancet.com+3pubmed.ncbi.nlm.nih.gov+3rscbayarea.com+3.Child cancer risk post-IVF is low but slightly elevated in some studies
Though one study found a 17% higher rate in IVF-conceived children, the overall cancer risk remains low med.umn.edu.
❓ Frequently Asked Questions
Q1: Will cancer treatment make me infertile?
Yes, chemotherapy and radiation can severely impact fertility—but options like IVF, cryopreservation, or ovarian transposition could preserve future fertility cancer.org+1mayoclinic.org+1.
Q2: What are my fertility preservation choices?
Egg or embryo freezing: Stimulates ovaries to retrieve and store eggs or embryos.
Ovarian transposition: Relocates ovaries out of radiation zones.
Ovarian tissue freezing: Preserves fertility for those not yet fully developed (e.g., young girls).
Sperm/testicular stem cell freezing: Used in young males pre-therapy cancer.org+1drjayanam.com+1.
Q3: Is there a cancer risk from IVF hormones?
Most large studies show no increased long-term risk for breast, ovarian, or uterine cancer due to fertility drugs thelancet.com+6pubmed.ncbi.nlm.nih.gov+6rscbayarea.com+6.
Q4: Can I still have biological children after surviving cancer?
Yes—patients using IVF after cancer may have slightly lower conception rates, but many become parents academic.oup.com.
Q5: Are IVF-conceived kids more prone to cancer?
Some data suggests a marginal rise in childhood liver tumors, but overall cancer risk is comparable to naturally conceived peers med.umn.edu+1pubmed.ncbi.nlm.nih.gov+1.
⏳ Timeline: From Conversation to Creation
Diagnosis: Oncologist and reproductive specialist assess impact on fertility.
Counseling: Discuss options including IVF, costs, timelines, success rates.
Preparation: Stimulate ovaries using hormones over 10–14 days .
Retrieval: Retrieve eggs (with anesthesia), optional embryo fertilization.
Preservation: Freeze eggs, embryos, or tissue for future use.
Treatment: Proceed with cancer therapy promptly.
Post-recovery family planning: Thaw and transfer embryos, or let tissues restore fertility. This may take months to years .
🏠 Impact on Daily Life
Emotional Stress & Hope: Fertility preservation offers agency amid fear, but involves anxiety, physical demands, and costs.
Financial Burden: Each IVF cycle costs thousands (typically $10k+). Cancer survivors also face long-term storage fees .
Physical Effects: Hormone therapy can cause side effects—bloating, mood swings, fatigue .
Relationships: Couples must make decisions under stress, navigate roles, and share uncertainty.
Long-Term Relief: Securing fertility may offer peace, reduce regret, and improve emotional recovery post-treatment.
🌍 Societal Significance
Oncofertility Recognizes Reproductive Rights in Cancer Care, emphasizing the importance of biological future.
Evolving Ethics & Accessibility: Many countries now include fertility preservation in cancer protocols. Clinics justify techniques historically developed for cancer patients .
Policy & Debate: In some regions, IVF access is threatened by legal shifts or cost barriers, particularly for disease-related fertility preservation .
Data Integrity & Safety: Cases like anonymous sperm donors lacking medical histories show the need for transparency in fertility medicine adelaidenow.com.au.
🎉 Wishes to Those Facing This Journey
“May your sense of choice bring comfort, your courage shine amid uncertainty, and your hope blossom into tomorrow’s joy. Your strength today is the foundation of your future.”
🧠 Observations & Best Practices
Start Early – Discuss fertility preservation immediately after diagnosis med.umn.edu+15cancer.org+15mayoclinic.org+15.
Multidisciplinary Team – Gather oncologists, fertility specialists, counselors for complete care.
Financial Planning – Explore insurance, grants, subsidies—public systems vary widely .
Transparency & Follow-up – Track health, reproductive plans, and data access for both patients and offspring .
Emotional Support – Build resilience with therapy, support groups, and partner/family communication.
✅ Conclusion: Fertility Tools in Cancer Care Are Empowering
The integration of IVF and fertility preservation into cancer treatment isn’t a luxury—it’s a lifeline of agency and hope. These options allow patients to control one part of their future amid uncertainty, reducing emotional burdens and enriching quality of life post-recovery.
This journey intertwines science with human resilience—offering a blueprint of hope, intimacy, and legacy in the face of illness.





I have been surfing online greater than three hours nowadays, yet I never found any interesting article like yours. It¦s beautiful worth enough for me. In my opinion, if all web owners and bloggers made excellent content as you probably did, the web can be a lot more helpful than ever before.